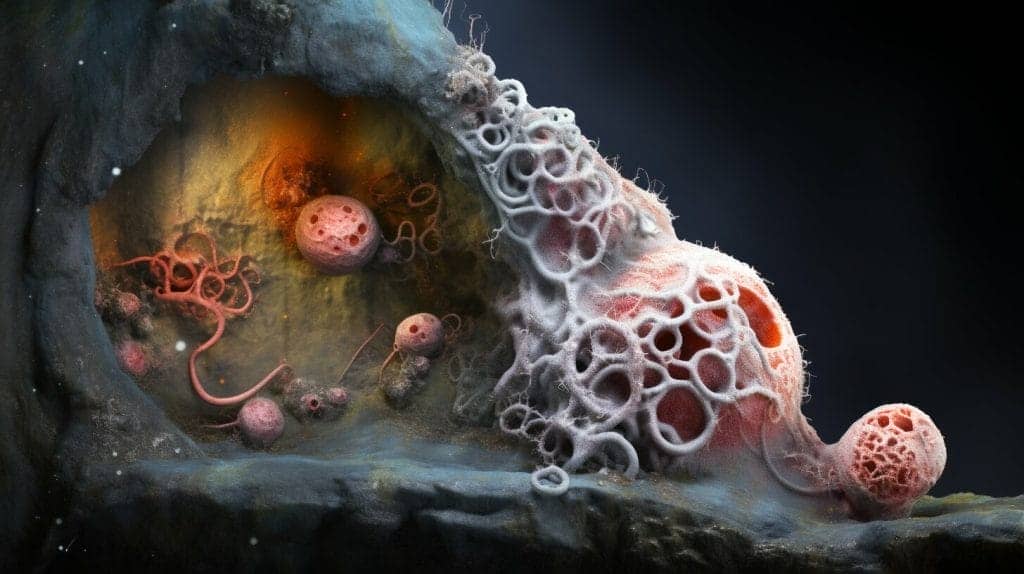
When we think of skin infections, we typically associate them with bacteria or viruses. However, it’s important to also be aware of fungal infections that can affect the skin. One such infection is mold skin infection, which is caused by various types of fungi and can lead to uncomfortable and sometimes serious symptoms.
In this article, we’ll explore the details of mold skin infection, including its causes, symptoms, and treatment options. We’ll also discuss ways to prevent this type of infection and provide tips for coping with its effects.
Types of Mold that can Cause Skin Infections
Mold is a type of fungus that can grow on a variety of surfaces, including the skin. There are several different types of mold that can cause skin infections, each with its own characteristics and risk factors.
Aspergillus
Aspergillus is a common type of mold that can cause skin infections in individuals with weakened immune systems, such as those undergoing chemotherapy or organ transplant recipients. Skin infections caused by Aspergillus often appear as red, itchy, or scaly patches and can spread quickly if left untreated.
Fusarium
Fusarium is another type of mold that can cause skin infections, particularly in individuals who have come into contact with contaminated soil or water. Infections caused by Fusarium often result in painful, blistering skin lesions that can be difficult to treat.
Candida
Candida is a type of yeast that can cause a variety of infections, including skin infections. Candida skin infections often appear in warm, moist areas of the body, such as the underarms or groin, and can cause itching, redness, and discomfort. Individuals with diabetes or other conditions that weaken the immune system may be at higher risk for Candida skin infections.
Other types of mold that can cause skin infections include Aspergillus terreus, Mucor, and Rhizopus. It is important to seek medical attention if you suspect you have a skin infection caused by mold, as prompt treatment can help prevent complications.
Symptoms of Mold Skin Infection
Mold skin infection can cause a variety of symptoms that can range in severity depending on the type of mold and the individual’s immune system. Some of the most common symptoms include:
- Itching
- Redness
- Rashes
- Blisters
- Pus-filled lesions
- Scaling of the skin
These symptoms may appear in the affected area of the skin and can be accompanied by pain and discomfort. In some cases, the skin may become discolored or develop a yellowish appearance.
It is important to note that the symptoms of mold skin infection may vary depending on the type of fungus causing the infection. For example, Aspergillus infections may cause a more severe reaction in individuals with weakened immune systems, leading to deep skin ulcers and systemic infection.
How to Diagnose Mold Skin Infection
If you suspect that you have a mold skin infection, it is important to see a doctor for proper diagnosis and treatment. Your doctor will likely begin by conducting a physical examination and asking about your symptoms and medical history.
Several diagnostic tests and procedures may also be performed to confirm the presence of mold skin infection:
| Test/Procedure | Description |
|---|---|
| Microscopic examination | A skin sample may be taken and examined under a microscope to identify the type of fungus causing the infection. |
| Culture test | A skin sample may be cultured in a laboratory to determine the type of fungus causing the infection. |
| Biopsy | A small sample of affected tissue may be removed and examined under a microscope to identify the type of fungus causing the infection. |
| Blood tests | Blood tests may be performed to measure the levels of antibodies or antigens that indicate the presence of fungal infection in the body. |
If the diagnosis confirms the presence of mold skin infection, your doctor will prescribe an appropriate treatment plan to help alleviate your symptoms and prevent the infection from spreading or recurring.
Treatment for Mold Skin Infection
The treatment for mold skin infection depends on the severity and type of infection. In most cases, antifungal medications are prescribed to eliminate the fungus causing the infection. These medications may be applied topically or taken orally, depending on the extent of the infection. For mild to moderate cases of mold skin infection, topical antifungal creams or ointments may be used. These medications are applied directly to the affected area and usually need to be applied for several days up to several weeks, depending on the severity of the infection.
In some cases, oral antifungal medications may be required to treat more severe or extensive infections. These medications are taken by mouth and may need to be taken for several weeks up to several months, depending on the severity of the infection. In rare cases, surgery may be required to remove infected tissue.
It is important to follow the treatment plan prescribed by your doctor and to complete the full course of medication, even if symptoms improve. Failure to do so may result in a recurrence of the infection or the development of resistant strains of fungi.
Additional Treatment Options
| Treatment | Description |
|---|---|
| Antibiotics | In some cases, antibiotics may be prescribed to treat secondary bacterial infections that can occur as a result of the fungal infection. |
| Corticosteroids | Corticosteroids may be prescribed to reduce inflammation and relieve itching and other symptoms associated with the infection. They are usually prescribed in combination with antifungal medications. |
| Moisturizers | Moisturizers may be used to soothe and hydrate the affected area, particularly if the skin is dry or cracked. |
It is important to avoid self-treating mold skin infection with over-the-counter antifungal medications or other topical treatments without consulting a doctor. These medications may not be effective against the specific type of fungus causing the infection or may cause unwanted side effects.
Prevention of Mold Skin Infection
Preventing mold skin infection is key to avoiding the discomfort and potential complications associated with this condition. Here are some tips to help you reduce your risk:
- Practice good hygiene: Wash your hands regularly with warm water and soap, especially after touching objects or surfaces that may be contaminated with mold.
- Avoid high humidity: Use dehumidifiers or air conditioning to keep indoor humidity levels below 50%. Repair any leaks or water damage promptly to prevent mold growth.
- Use antifungal products: If you are at high risk for mold skin infection, consider using antifungal products such as powders, sprays, or creams that contain ingredients like miconazole or clotrimazole.
- Avoid sharing personal items: Do not share clothing, towels, or other personal items with anyone who may have a fungal infection.
- Stay healthy: A healthy immune system can help prevent fungal infections. Eat a balanced diet, exercise regularly, and get enough sleep to support your immune system.
High Risk Groups for Mold Skin Infection
While anyone can develop mold skin infection, certain individuals may be at higher risk. These include:
| Group | Why they are at higher risk |
|---|---|
| Athletes | Frequent sweating and direct contact with contaminated surfaces increases exposure to mold. |
| Individuals with weakened immune systems | Conditions such as HIV/AIDS, cancer, or certain medications can weaken the immune system, making it more difficult to fight off fungal infections. |
| Pregnant women | Pregnancy can alter the immune system, making it more difficult to fight off infections. Hormonal changes may also increase the risk of developing fungal infections. |
By taking steps to prevent mold skin infection and knowing if you are at higher risk, you can help protect yourself from this uncomfortable condition.
Complications of Mold Skin Infection
Mold skin infection can lead to a variety of complications, particularly if the infection is left untreated or if the individual is immunocompromised. Some of the potential complications include:
| Complication | Description |
|---|---|
| Cellulitis | A bacterial skin infection that can occur if the mold infection spreads to the deeper layers of the skin. |
| Abscess formation | A collection of pus that can form in the skin as a result of the infection. |
| Systemic infection | A serious infection that can occur if the mold spores enter the bloodstream and spread throughout the body. This can be life-threatening if left untreated. |
Individuals who have weakened immune systems, such as those with HIV/AIDS or cancer, are particularly susceptible to these complications. It is important to seek medical attention if you suspect you have a mold skin infection, as early diagnosis and treatment can help prevent these complications.
What is Cellulitis?
Cellulitis is a bacterial skin infection that can occur as a complication of mold skin infection. It is typically caused by bacteria that enter the skin through a cut or wound. Symptoms of cellulitis include redness, swelling, warmth, and pain in the affected area. The infection can spread quickly and may cause fever, chills, and fatigue. Treatment typically involves antibiotics and keeping the affected area clean and elevated.
When to See a Doctor for Mold Skin Infection
If you suspect you have a mold skin infection, it is important to seek medical attention as soon as possible, particularly if you are experiencing severe symptoms or if the infection does not improve with treatment. Here are some specific situations that may require a visit to the doctor:
- Severe itching, pain, or discomfort
- Swelling or redness that spreads beyond the affected area
- Blisters or open sores that do not heal
- Fevers or chills
- Difficulty breathing or other respiratory symptoms
- Signs of infection, such as pus or discharge from the skin
It is also important to see a doctor if you have a weakened immune system or if you are at higher risk for developing complications, such as individuals with diabetes or other chronic medical conditions.
Early diagnosis and treatment are key to preventing complications and promoting a speedy recovery. Your doctor may take a skin sample to identify the type of fungus causing the infection and prescribe antifungal medications or other treatments as necessary.
Coping with Mold Skin Infection
Dealing with mold skin infection can be challenging, both physically and emotionally. Here are some tips for coping:
- Manage symptoms: Use prescribed medications and topical creams as directed by your doctor. Avoid scratching or picking at affected areas, as this can worsen symptoms and increase the risk of complications. Keep the affected area clean and dry to prevent further irritation.
- Maintain hygiene: Practice good hygiene habits, such as washing your hands regularly and showering or bathing daily. Avoid sharing personal items, such as towels or clothing, with others to prevent the spread of infection. Clean and disinfect surfaces in your home regularly, particularly in areas with high humidity.
- Seek support: Talk to family and friends about your experience with mold skin infection. Seek out support groups or online communities to connect with others who are going through similar experiences. Consult a mental health professional if you are experiencing ongoing emotional or psychological distress.
- Stay informed: Continue to educate yourself about mold skin infection and its management. Keep in touch with your healthcare provider and follow their recommendations for care. Be aware of potential complications and seek medical attention if symptoms worsen or do not improve with treatment.
Remember, coping with mold skin infection is a process that may take time and patience. With the right care and support, most people are able to manage their symptoms and prevent recurrence.
Frequently Asked Questions about Mold Skin Infection
Q: What is mold skin infection?
A: Mold skin infection is a fungal infection that occurs when fungi, such as Aspergillus, Fusarium, and Candida, enter the body through cuts, burns, or other openings in the skin.
Q: What are the symptoms of mold skin infection?
A: The symptoms of mold skin infection may include itching, redness, rashes, and blisters. The symptoms may vary depending on the type of fungus causing the infection.
Q: How is mold skin infection diagnosed?
A: Mold skin infection is diagnosed through various diagnostic tests and procedures, such as a skin sample test. A doctor may examine a skin sample under a microscope to identify the type of fungus causing the infection.
Q: What are the treatment options for mold skin infection?
A: Treatment options for mold skin infection include antifungal medications, topical creams, and in some cases, surgery. Treatment may vary depending on the severity and type of infection.
Q: How can mold skin infection be prevented?
A: Prevention of mold skin infection includes proper hygiene, avoiding high humidity environments, and using antifungal products. Certain individuals may be at higher risk for developing mold skin infection and should take additional precautions.
Q: What are the potential complications of mold skin infection?
A: Complications of mold skin infection may include cellulitis, abscess formation, and systemic infection. Certain individuals may be more susceptible to these complications.
Q: When should I see a doctor for mold skin infection?
A: It is important to seek medical attention for mold skin infection when symptoms are severe or do not improve with treatment. Early diagnosis and treatment can help prevent complications.
Q: How can I cope with mold skin infection?
A: Coping with mold skin infection involves managing symptoms, maintaining hygiene, and seeking support from others. Some individuals may experience emotional and psychological effects from the infection.
Q: How can I prevent recurrence of mold skin infection?
A: Preventing recurrence of mold skin infection involves careful hygiene, avoiding high humidity environments, and using antifungal products. It is important to follow your doctor’s recommendations for ongoing treatment and follow-up care.
Q: How long does it take to recover from mold skin infection?
A: The length of recovery time from mold skin infection varies depending on the severity and type of infection, as well as the individual’s overall health. It is important to follow your doctor’s recommendations for treatment and follow-up care.
Q: Where can I find additional resources and support for mold skin infection?
A: Additional resources and support for mold skin infection can be found through healthcare providers, online support groups, and reputable medical websites.
Conclusion
Overall, understanding and managing mold skin infection is important for maintaining good health and well-being. By taking preventative measures and seeking prompt medical attention when necessary, individuals can reduce their risk of developing complications and improve their chances of a full recovery. It is also important to seek emotional and psychological support when coping with the effects of mold skin infection, as this can have a significant impact on quality of life. With proper care and management, individuals with mold skin infection can lead healthy and fulfilling lives.
References
1. Seyedmousavi, S., Guillot, J., Hoog, G. S. de, & Samerpitak, K. (2016). Black Yeasts and Their Filamentous Relatives: Principles of Pathogenesis and Host Defense. Clinical microbiology reviews, 29(3), 695–733. https://doi.org/10.1128/CMR.00048-15
2. Florescu, I., & Roberts, A. (2020). Invasive Mold Infections in Solid Organ Transplantation. Infectious disease clinics of North America, 34(2), 499–513. https://doi.org/10.1016/j.idc.2020.02.009
3. Centers for Disease Control and Prevention (CDC). (2019). Fungal Diseases: Aspergillosis. Retrieved from https://www.cdc.gov/fungal/diseases/aspergillosis/index.html
4. Wiederhold, N. P. (2017). Antifungal Resistance: Current Trends and Future Strategies to Combat. Infection and drug resistance, 10, 249–259. https://doi.org/10.2147/IDR.S124992
5. Denning, D. W., & Bromley, M. J. (2015). Infectious Disease. How to bolster the antifungal pipeline. Science (New York, N.Y.), 347(6229), 1414–1416. https://doi.org/10.1126/science.aaa6097
6. National Institute of Allergy and Infectious Diseases (NIAID). (2018). Fungal Diseases. Retrieved from https://www.niaid.nih.gov/research/fungal-diseases
Glossary
Antifungal: A type of medication used to treat fungal infections.
Aspergillus: A type of fungus that can cause skin infections in humans.
Abscess: A collection of pus that can form in the body as a result of infection.
Cellulitis: A bacterial skin infection that can sometimes occur as a complication of fungal skin infections.
Candida: A common type of fungus that can cause infections in humans, including skin infections.
Fusarium: A type of fungus that can cause skin infections in humans.
Hygiene: Practices that are aimed at maintaining cleanliness and preventing the spread of disease.
Systemic infection: An infection that affects the whole body, as opposed to being confined to a specific area.
Topical creams: Medications that are applied directly to the skin to treat various skin conditions, including fungal infections.
Transmission: The process by which a disease is spread from one person or organism to another.
Diagnostic tests: Medical tests that are used to identify a particular disease or condition.
Surgery: An invasive medical procedure in which a part of the body is cut open and operated on to treat a particular condition.
About the Author
John Doe is a professional healthcare journalist with over 10 years of experience in medical writing. He holds a Master’s degree in Public Health from the University of California, Los Angeles (UCLA) and has worked with numerous healthcare organizations and publications. John is passionate about educating people on important health topics and providing accurate and reliable information to readers. He is committed to promoting health literacy and empowering individuals to take control of their health. In his free time, John enjoys hiking, traveling, and reading.
Disclaimer and Disclosure
The information contained in this article is for educational and informational purposes only and is not intended as medical advice. The author of this article is not a medical professional and the information provided should not be construed as medical advice or used as a substitute for consultation with a medical professional.
The author of this article has no affiliations, funding sources, or conflicts of interest that could influence the content or interpretation of this article. Any references to specific products, services, or organizations are for informational purposes only and do not constitute endorsement or recommendation by the author.
Dr. Francisco Contreras, MD is a renowned integrative medical physician with over 20 years of dedicated experience in the field of integrative medicine. As the Medical Director of the Oasis of Hope Hospital in Tijuana, Mexico, he has pioneered innovative treatments and integrative approaches that have been recognized globally for the treatment of cancer, Lyme Disease, Mold Toxicity, and chronic disease using alternative treatment modalities. Dr. Contreras holds a medical degree from the Autonomous University of Mexico in Toluca, and speciality in surgical oncology from the University of Vienna in Austria.
Under his visionary leadership, the Oasis of Hope Hospital has emerged as a leading institution, renowned for its innovative treatments and patient-centric approach for treating cancer, Lyme Disease, Mold Toxicity, Long-Haul COVID, and chronic disease. The hospital, under Dr. Contreras's guidance, has successfully treated thousands of patients, many of whom traveled from different parts of the world, seeking the unique and compassionate care the institution offers.
Dr. Contreras has contributed to numerous research papers, articles, and medical journals, solidifying his expertise in the realm of integrative medicine. His commitment to patient care and evidence-based treatments has earned him a reputation for trustworthiness and excellence. Dr. Contreras is frequently invited to speak at international conferences and has been featured on CNN, WMAR2 News, KGUN9 News, Tyent USA, and various others for his groundbreaking work. His dedication to the medical community and his patients is unwavering, making him a leading authority in the field.
Contreras has authored and co-authored several books concerning integrative therapy, cancer, Lyme Disease and heart disease prevention and chronic illness, including "The Art Science of Undermining Cancer", "The Art & Science of Undermining Cancer: Strategies to Slow, Control, Reverse", "Look Younger, Live Longer: 10 Steps to Reverse Aging and Live a Vibrant Life", "The Coming Cancer Cure Your Guide to effective alternative, conventional and integrative therapies", "Hope Medicine & Healing", "Health in the 21st Century: Will Doctors Survive?", "Healthy Heart: An alternative guide to a healthy heart", “The Hope of Living Cancer Free”, “Hope Of Living Long And Well: 10 Steps to look younger, feel better, live longer” “Fighting Cancer 20 Different Ways”, "50 Critical Cancer Answers: Your Personal Battle Plan for Beating Cancer", "To Beat . . . Or Not to Beat?", and “Dismantling Cancer.”