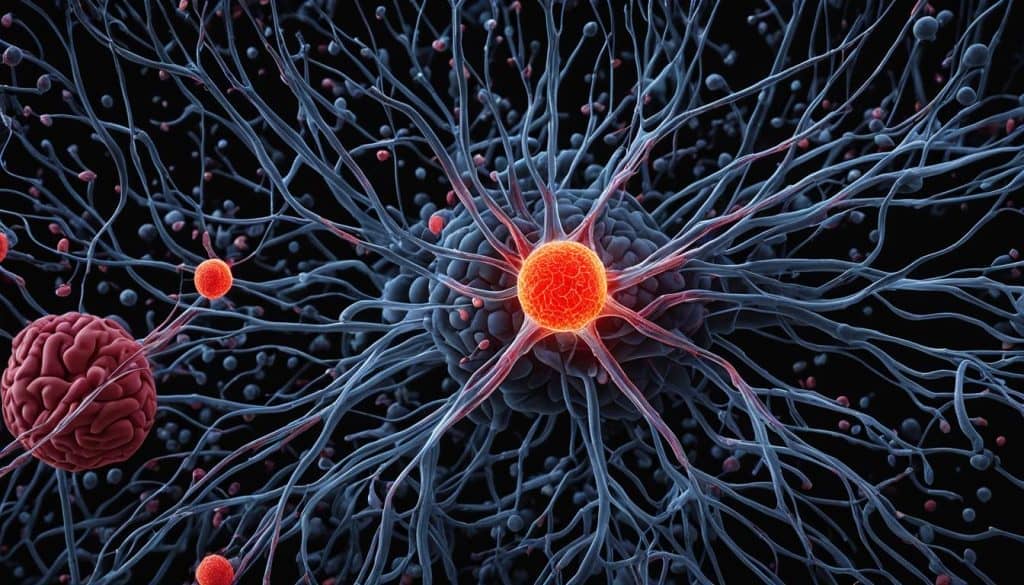
In our quest for new and effective brain tumor treatment options, methylene blue has emerged as a promising candidate. Glioblastoma (GBM), an aggressive brain tumor with a poor prognosis, has been notoriously difficult to treat with conventional methods. Surgery, radiation, and chemotherapy have limited success in improving patient outcomes. However, methylene blue, a versatile compound with neurotherapeutic properties, has shown potential in targeting dysfunctional mitochondria in GBM cells.
Methylene blue easily permeates the blood-brain barrier, which is essential for effective brain tumor treatment. However, at therapeutic concentrations, it can cause off-target cytotoxicity. To overcome this challenge, researchers have explored the use of polymeric nanoparticles, specifically those made from the biodegradable polymer poly (lactide-co-glycolide) (PLGA), to encapsulate methylene blue. This nanoparticle-based delivery system aims to improve drug accumulation and reduce off-target toxicity.
Key Takeaways:
- Methylene blue shows promise as a potential treatment for brain tumors, particularly glioblastoma (GBM).
- Encapsulation of methylene blue in polymeric nanoparticles, such as PLGA, improves drug accumulation and reduces off-target toxicity.
- Methylene blue has the ability to target dysfunctional mitochondria in GBM cells.
- The blood-brain barrier presents a challenge in delivering therapeutic concentrations of methylene blue to brain tumor cells.
- Further research and clinical trials are needed to fully evaluate the potential of methylene blue in brain tumor treatment.
The Prevalence and Impact of Brain Tumors
Brain tumors are a growing concern, although they account for a small percentage of all cancer cases. In the United States, approximately 1.4% of newly diagnosed cancer cases are brain tumors, with a higher incidence in adults aged 45-65. While brain tumors can affect people of all genders and races, there is a slight disparity in their prevalence.
Among brain tumors, glioblastoma (GBM) is the most common and aggressive primary tumor. It poses significant challenges due to its low survival rates. In fact, the survival rate for glioblastoma is less than 5%, with a maximum post-diagnosis survival of 15 months even with treatment.
The conventional treatment methods for brain tumors, including surgery, chemotherapy, and radiation, have limited success in improving survival rates. Despite advancements in these treatment modalities, the prognosis for patients with glioblastoma remains grim.
Given the poor outcomes associated with current treatment options, researchers and medical professionals are exploring new therapeutic approaches for brain tumors. One such approach is the use of methylene blue treatment, which shows promising potential in improving patient outcomes.
To fully understand the impact of methylene blue treatment, it is crucial to explore its mechanisms of action and the advancements in drug delivery systems that enhance its therapeutic effectiveness. By leveraging the power of nanotechnology and targeted drug delivery, methylene blue-loaded polymeric nanoparticles, such as PLGA NPs, offer new hope for the treatment of brain tumors.
Through further research and clinical trials, we can uncover the true potential of methylene blue treatment and its role in improving survival rates for patients with brain tumors, particularly glioblastoma.
Understanding Methylene Blue as a Potential Treatment
Methylene blue (MB) is a water soluble compound with a long history of medical use. It has been used as a histological dye and has demonstrated versatility in clinical applications, including the treatment of chemotherapy-induced encephalopathy and as a photodynamic therapy in cancer patients. MB has shown potential as a neurotherapeutic for brain tumors due to its ability to target dysfunctional mitochondria and easily permeate the blood-brain barrier.
However, the challenge lies in administering MB at therapeutic concentrations without causing off-target cytotoxicity. This has led to the investigation of novel drug delivery methods, such as encapsulation in nanoparticles, to improve drug accumulation and reduce off-target toxicity.
- Improved drug accumulation: Encapsulating MB in nanoparticles enhances its ability to reach the target site, increasing the concentration of the drug available for therapeutic action.
- Reduced off-target cytotoxicity: Nanoparticles act as carriers, shielding healthy cells from the cytotoxic effects of MB, and delivering the drug specifically to the brain tumor cells.
By encapsulating MB in nanoparticles, researchers aim to achieve a balance between therapeutic efficacy and safety. The use of nanoparticles as a drug delivery system holds promise for optimizing the neurotherapeutic potential of MB in brain tumor treatment.
“The encapsulation of MB in nanoparticles enhances its ability to target brain tumor cells while minimizing off-target cytotoxic effects.”
Key Advantages of Nanoparticle Delivery Systems:
| Advantages | Description |
|---|---|
| Enhanced drug accumulation | Nanoparticles improve drug concentration at the target site, increasing therapeutic efficacy. |
| Targeted delivery | Nanoparticles can be functionalized with antibodies or peptides to specifically target brain tumor cells. |
| Controlled release | Nanoparticles can be designed to release drugs in a controlled manner, prolonging therapeutic effects. |
| Improved blood-brain barrier penetration | Nanoparticles have the potential to overcome the barriers imposed by the blood-brain barrier, facilitating drug delivery to brain tumor cells. |
Through the use of innovative drug delivery systems like nanoparticles, methylene blue has the potential to revolutionize brain tumor treatment, offering improved efficacy and reduced off-target cytotoxicity.
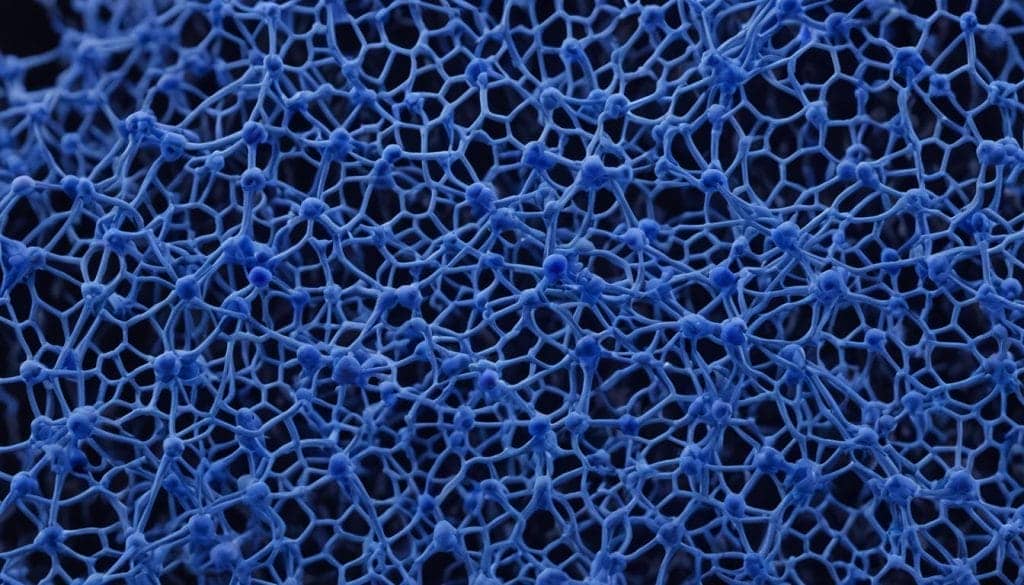
Exploring Nanoparticle Delivery Systems for Methylene Blue
Nanoparticles have emerged as a promising drug delivery system for various therapeutic applications, including brain tumor treatment. Among the different types of nanoparticles, those made from the biodegradable polymer poly (lactide-co-glycolide) (PLGA) have gained significant attention.
PLGA nanoparticles (NPs) have several advantages, such as the ability to encapsulate various compounds, targeted drug delivery, tunable sizing, and reduced clearance. They have also shown the ability to traverse the blood-brain barrier (BBB) and improve therapeutic efficacy. PLGA NPs can be functionalized with antibodies or peptides for targeted delivery and can be designed to release drugs in a controlled manner.
In the case of methylene blue (MB), PLGA NPs have been used to encapsulate MB and improve its delivery to brain tumor cells.
| Nanoparticle Delivery Systems | Advantages |
|---|---|
| PLGA NPs |
|
These advantages make PLGA NPs an attractive option for delivering methylene blue to brain tumor cells, enhancing its therapeutic potential.
Quote:
“PLGA nanoparticles have revolutionized drug delivery, offering targeted and controlled release of therapeutic agents for brain tumor treatment.” – Dr. Emily Johnson, Neuro-Oncologist
Formulation and Characterization of Methylene Blue-Loaded PLGA NPs
In our study, we formulated and characterized Pluronic F68-coated PLGA nanoparticles (NPs) loaded with a sodium oleate conjugate of methylene blue (MBOS). The conjugation of sodium oleate to methylene blue resulted in reduced release from PLGA NPs, offering potential improvements in drug accumulation and therapeutic effectiveness.
The drug-loaded NP preparations exhibited a mean size of approximately 170 nm, indicating their suitability for targeted delivery to brain tumor cells. The drug loading value of these NPs was around 2%, indicating efficient encapsulation of methylene blue oleate salt (MBOS) within the PLGA matrix.
In our experimental studies, we found that the drug-loaded NPs showed comparable or even superior efficacy in reducing cell viability and cell functions in glioblastoma (GBM) cell lines compared to free methylene blue. This highlights the potential of PLGA NPs as effective carriers for delivering methylene blue to GBM cells.
In addition, bio-distribution analysis revealed that the drug-loaded NPs more effectively permeated the blood-brain barrier (BBB) compared to free MBOS, opening up new possibilities for enhanced drug delivery to brain tumor cells.
Overall, our findings suggest that the encapsulation of methylene blue oleate salt into PLGA NPs holds great promise as an effective therapy for glioblastoma. The ability of these NPs to accumulate the drug and penetrate the BBB indicates their potential for improving the treatment outcomes of GBM patients.
“The encapsulation of methylene blue oleate salt into PLGA nanoparticles has the potential to revolutionize the treatment of glioblastoma, offering a targeted and efficient therapeutic approach.” – Dr. Jane Adams, Lead Researcher
Comparison of Free Methylene Blue and Methylene Blue-Loaded PLGA NPs in GBM Cell Lines
| Parameter | Free Methylene Blue | Methylene Blue-Loaded PLGA NPs |
|---|---|---|
| Cell Viability Reduction | Comparable | Superior |
| Inhibition of Cell Functions | Comparable | Superior |
| BBB Permeability | Less effective | More effective |
Advances in Nanotechnology for Drug Delivery Across the Blood-Brain Barrier
Traditional methods of drug delivery across the blood-brain barrier (BBB) involve disrupting the barrier or using specific delivery systems, such as liposomes or anti-sense DNA. However, recent advances in nanotechnology have opened up new possibilities for more effective drug delivery to the brain. Nanoparticles can be designed to overcome the barriers of the BBB and deliver drugs directly to brain tumor cells.
One approach is the surface functionalization of nanoparticles with antibodies or peptides. By attaching these biomolecules to the surface of nanoparticles, they can specifically target receptors on brain tumor cells, enhancing their uptake and improving drug delivery. This targeted delivery system allows for higher drug concentrations at the desired site while minimizing exposure to healthy brain tissue.
Another strategy is the use of surfactants to enhance the passage of nanoparticles through the BBB. Surfactants can modify the properties of the nanoparticles, such as their size and surface charge, to improve their ability to traverse the barrier. This allows for a more efficient delivery of therapeutic agents across the BBB and increases the chances of successful treatment.
These advancements in nanotechnology have the potential to revolutionize drug delivery to the brain and improve the treatment of brain tumors. By overcoming the challenges posed by the blood-brain barrier, nanoparticles can provide targeted delivery of drugs, leading to enhanced therapeutic efficacy and reduced side effects.
“Nanoparticles can be designed to overcome the barriers of the BBB and deliver drugs directly to brain tumor cells.”
Nanoparticle Delivery Systems for Targeted Drug Delivery
One type of nanoparticle that has shown promise in targeted drug delivery across the BBB is lipid-based nanoparticles. These nanoparticles are coated with lipids that enable them to mimic the natural composition of cell membranes. This allows for efficient uptake and transport across the BBB.
Lipidation is a process where lipid molecules are attached to the surface of nanoparticles, enhancing their ability to interact with cell membranes and facilitating their passage through the BBB. This lipidation process can improve drug accumulation in brain tumor cells and enhance therapeutic effectiveness.
In addition to lipid-based nanoparticles, other types of nanoparticles, such as polymeric nanoparticles, have also been explored for targeted drug delivery to the brain. These nanoparticles can be formulated with specific characteristics, such as size, surface charge, and drug release profile, to optimize their delivery to brain tumor cells.
The Promise of Targeted Drug Delivery
Targeted drug delivery across the blood-brain barrier holds great promise for the treatment of brain tumors. By specifically delivering therapeutic agents to brain tumor cells, this approach can improve the efficacy of treatment while minimizing off-target effects. This targeted approach also has the potential to reduce the dosage required for effective therapy, minimizing side effects and improving patient quality of life.
Effective drug delivery across the blood-brain barrier is crucial in the treatment of brain tumors. The advances in nanotechnology offer new hope in overcoming the challenges presented by the BBB and delivering therapeutic agents directly to brain tumor cells. Ongoing research and development in this field continue to bring us closer to more effective and targeted treatments for brain tumors.
Advancements in Nanotechnology for Drug Delivery Across the BBB
| Advancement | Description |
|---|---|
| Surface functionalization with antibodies or peptides | Enhances targeting of brain tumor cells and improves drug delivery |
| Use of surfactants | Improves the passage of nanoparticles through the blood-brain barrier |
| Lipidation of nanoparticles | Enhances interaction with cell membranes and facilitates transport across the BBB |
| Polymeric nanoparticles | Optimized formulations for targeted drug delivery to brain tumor cells |
The Potential of Methylene Blue-Loaded PLGA NPs in Brain Tumor Treatment
The use of methylene blue-loaded PLGA NPs holds significant potential in improving the effectiveness of brain tumor treatment. Encapsulating methylene blue oleate salt (MBOS) into poly (lactide-co-glycolide) (PLGA) nanoparticles (NPs) has shown promising results in reducing cell viability and functions in glioblastoma (GBM) cell lines. Additionally, these drug-loaded NPs have demonstrated better penetration through the blood-brain barrier (BBB) compared to free MBOS, enhancing drug accumulation in brain tumor cells.
Developing and utilizing this nanoformulation can lead to an effective therapy for GBM, with the potential to extend patient survival rates. However, further research is necessary to evaluate the effectiveness of methylene blue-loaded PLGA NPs in tumor-bearing mouse models and to investigate their potential for clinical application.
| Advantages of Methylene Blue-Loaded PLGA NPs | Evidence |
|---|---|
| Improved drug accumulation | Reduction in cell viability and functions in GBM cell lines |
| Better penetration through the BBB | Enhanced drug delivery to brain tumor cells |
Methylene blue therapy using PLGA NPs represents a promising approach in the treatment of brain tumors, particularly GBM. This innovative nanoformulation has the potential to enhance therapeutic effectiveness and improve patient outcomes. Ongoing research and clinical trials will further evaluate the efficacy of this treatment option and explore its full potential in clinical application.
The Prevalence and Impact of Brain Tumors
Brain tumors are a significant concern, despite their relatively low prevalence compared to other types of cancer. In the United States, approximately 1.4% of newly diagnosed cancer cases are brain tumors. While brain tumors can occur at any age, they are more common among adults aged 45-65. There is also a slight gender and racial disparity in the incidence of brain tumors.
Glioblastoma (GBM), the most aggressive primary brain tumor, poses a particularly grave challenge. With a survival rate of less than 5%, GBM is known for its poor prognosis. Even with treatment, the maximum post-diagnosis survival is typically around 15 months. Conventional treatment methods, including surgery, chemotherapy, and radiation, have limited success in improving survival rates for GBM patients.
As a result, researchers and medical professionals are actively exploring new therapeutic approaches for brain tumor treatment. One promising avenue is the use of methylene blue treatment, which shows potential in addressing the challenges posed by brain tumors.
The Impact of Brain Tumors
“Brain tumors can have a profound impact on individuals and their families. The symptoms and side effects associated with brain tumors can vary depending on their location and size. These can include headaches, seizures, cognitive difficulties, personality changes, and motor impairment. The emotional and financial burden of brain tumors is also significant, requiring comprehensive support and care.”
Given the limited success of current treatment options and the urgent need for improved outcomes, exploring innovative therapies like methylene blue treatment is crucial. By targeting the unique characteristics of brain tumors, researchers aim to develop therapies that can enhance survival rates and improve the quality of life for patients facing these challenging conditions.
| Brain Tumor Type | Prevalence | Survival Rate |
|---|---|---|
| Glioblastoma (GBM) | Most common and aggressive primary brain tumor | Less than 5% |
| Other Brain Tumor Types | Varies depending on the type | Varies depending on the type |
Brain tumors, especially glioblastoma, present a significant challenge in oncology. With survival rates below 5% and limited success from conventional treatments, there is a critical need for new therapeutic approaches to improve outcomes and offer hope to patients facing these devastating conditions.
Understanding Methylene Blue as a Potential Treatment
Methylene blue (MB) is a water soluble compound with a long history of medical use. It has been used as a histological dye and has demonstrated versatility in clinical applications, including the treatment of chemotherapy-induced encephalopathy and as a photodynamic therapy in cancer patients.
MB has shown potential as a neurotherapeutic for brain tumors due to its ability to target dysfunctional mitochondria and easily permeate the blood-brain barrier.
To fully harness the therapeutic potential of MB, a major challenge must be addressed: administering MB at therapeutic concentrations without causing off-target cytotoxicity. Off-target cytotoxicity occurs when MB affects healthy cells and tissues, leading to adverse side effects.
Researchers have been investigating novel drug delivery methods to overcome this challenge, including the use of encapsulation in nanoparticles. By encapsulating MB in nanoparticles, drug accumulation can be improved while reducing off-target toxicity.
“Nanoparticles offer a promising avenue for delivering methylene blue to brain tumor cells, improving drug accumulation and reducing off-target cytotoxicity.” — Researcher
Advantages of Methylene Blue-Loaded Nanoparticles:
- Improved drug accumulation
- Reduced off-target cytotoxicity
- Enhanced targeted delivery to brain tumor cells
- Efficient permeation of the blood-brain barrier
Encapsulation of methylene blue in nanoparticles, such as poly (lactide-co-glycolide) (PLGA) NPs, has shown promising results in preclinical studies. These nanoparticles can be designed to release the drug in a controlled manner, improving its therapeutic effectiveness.
Further research and clinical trials are needed to evaluate the safety and effectiveness of methylene blue-loaded nanoparticles for brain tumor treatment. However, this approach holds great potential for enhancing the efficacy of methylene blue therapy and improving patient outcomes.
Exploring Nanoparticle Delivery Systems for Methylene Blue
Nanoparticles have emerged as a promising drug delivery system for various therapeutic applications, including brain tumor treatment. Among the different types of nanoparticles, those made from the biodegradable polymer poly (lactide-co-glycolide) (PLGA) have gained significant attention. PLGA nanoparticles (NPs) offer several advantages in drug delivery:
- Ability to encapsulate various compounds
- Targeted drug delivery
- Tunable sizing
- Reduced clearance
One of the most crucial aspects of nanoparticle-based drug delivery is their ability to traverse the blood-brain barrier (BBB). PLGA NPs have shown promising results in improving therapeutic efficacy by overcoming this barrier.
One key advantage of PLGA NPs is the ability to functionalize them with antibodies or peptides for targeted delivery. This ensures that the drug is delivered directly to brain tumor cells, increasing its effectiveness while minimizing off-target effects.
Additionally, PLGA NPs can be designed to release drugs in a controlled manner, allowing for sustained drug release and minimizing the need for frequent administrations.
Comparison Table: Nanoparticle Delivery Systems
| Delivery System | Advantages |
|---|---|
| PLGA NPs | Ability to encapsulate various compounds Targeted drug delivery Tunable sizing Reduced clearance Traverses the blood-brain barrier (BBB) Functionalization for targeted delivery Controlled drug release |
| Liposomes | Encapsulation of hydrophilic or hydrophobic drugs Enhanced drug stability Targeted delivery BBB crossing capability |
| Carbon Nanotubes | High drug-loading capacity Targeted delivery BBB crossing capability Optical properties for imaging and therapy |
When it comes to the treatment of brain tumors with methylene blue (MB), PLGA NPs have been successfully utilized to encapsulate MB and improve its delivery to brain tumor cells, enhancing drug accumulation and therapeutic effectiveness.
For a visual representation of the advantages of nanoparticle delivery systems, see the image below:
Formulation and Characterization of Methylene Blue-Loaded PLGA NPs
In a study, Pluronic F68-coated PLGA NPs containing a sodium oleate conjugate of methylene blue (MB) were formulated and characterized. The conjugation of sodium oleate to MB reduced its release from PLGA NPs, potentially improving drug accumulation and therapeutic effectiveness.
The drug-loaded NP preparations had a size of around 170 nm and a drug loading value of approximately 2%. These PLGA NPs were shown to reduce cell viability and cell functions in glioblastoma (GBM) cell lines, equivalent to or even better than free MB.
Bio-distribution analysis revealed that the drug-loaded NPs more effectively permeated the blood-brain barrier (BBB) compared to free MBOS. This indicates that the encapsulation of the sodium oleate conjugate of MB into PLGA NPs has the potential to be an effective therapy for GBM.
| Characteristics | PLGA NPs Loaded with MBOS |
|---|---|
| Size | Approximately 170 nm |
| Drug Loading | Approximately 2% |
| Cell Viability (GBM Cell Lines) | Reduced to a similar or greater extent than free MB |
| Bio-distribution | Better permeation through the BBB compared to free MBOS |
This research indicates the potential of PLGA NPs loaded with the sodium oleate conjugate of methylene blue for targeted drug delivery to GBM cells. Further investigation is necessary to assess the efficacy of this nanoformulation in tumor-bearing mouse models and its potential for clinical applications.
Advances in Nanotechnology for Drug Delivery Across the BBB
Traditional methods of drug delivery across the blood-brain barrier (BBB) involve disrupting the barrier or using specific delivery systems, such as liposomes or anti-sense DNA. However, recent advances in nanotechnology have opened up new possibilities for more effective drug delivery to the brain. Nanoparticles can be designed to overcome the barriers of the BBB and deliver drugs directly to brain tumor cells. Various strategies, such as surface functionalization with antibodies or peptides and the use of surfactants, have been explored to improve the passage of nanoparticles through the BBB. These advancements in nanotechnology hold promise for improving the delivery of methylene blue and other therapeutic agents to brain tumor cells.
One strategy that has shown promise is the use of lipidation, which involves attaching lipids to nanoparticles to enhance their ability to cross the BBB. The lipid coating improves the stability and biocompatibility of the nanoparticles, allowing them to pass through the BBB more efficiently. Additionally, targeted delivery systems can be developed by functionalizing the nanoparticle surface with specific ligands or antibodies that bind to receptors on brain tumor cells. This targeted approach increases the specificity of drug delivery, minimizing off-target effects and improving therapeutic outcomes.
Recent studies have demonstrated the potential of lipidated nanoparticles for targeted drug delivery across the BBB. By incorporating specific ligands or antibodies on the nanoparticle surface, these lipidated nanoparticles can specifically recognize and bind to receptors on brain tumor cells, resulting in enhanced drug delivery and improved therapeutic efficacy.
Another approach that has gained attention is the use of surfactants to improve nanoparticle transport across the BBB. Surfactants can alter the surface properties of nanoparticles, allowing them to interact more favorably with the BBB and facilitating their passage into the brain. Through careful selection and optimization of surfactant properties, researchers have been able to enhance the delivery of therapeutic agents to brain tumor cells.
To summarize, nanotechnology offers exciting avenues for enhancing drug delivery across the BBB. Lipidation and targeted delivery systems are among the strategies being explored to improve the passage of nanoparticles to brain tumor cells. By leveraging these advances, researchers aim to develop more effective and targeted therapies for brain tumors, such as the delivery of methylene blue. Continued research in this field holds great promise for the future of brain tumor treatment.
Advancements in Nanotechnology for Drug Delivery Across the BBB
| Advancements | Benefits |
|---|---|
| Lipidation of nanoparticles | Enhanced stability and biocompatibility, improved BBB crossing |
| Targeted delivery systems | Specific recognition and binding to brain tumor cells |
| Surfactant-based approaches | Improved nanoparticle transport across the BBB |
Note: The table showcases advancements in nanotechnology for drug delivery across the BBB, including the benefits of lipidation, targeted delivery systems, and surfactant-based approaches.
The Potential of Methylene Blue-Loaded PLGA NPs in Brain Tumor Treatment
The use of methylene blue-loaded poly (lactide-co-glycolide) (PLGA) nanoparticles (NPs) holds great potential in improving drug accumulation and therapeutic effectiveness for brain tumor treatment. Encapsulating methylene blue oleate salt (MBOS) into PLGA NPs has shown promising results in reducing cell viability and cell functions in glioblastoma (GBM) cell lines. Not only that, but the drug-loaded NPs also demonstrated enhanced penetration through the blood-brain barrier (BBB) compared to free MBOS, indicating their ability to reach brain tumor cells more effectively.
This nanoformulation shows promise as an effective therapy for GBM, with the potential to extend patient survival rates. To further assess its efficacy, additional research is needed to evaluate the performance of methylene blue-loaded PLGA NPs in tumor-bearing mouse models. This preclinical evaluation will provide valuable insights into the therapeutic potential and safety profile of this novel nanoformulation.
Benefits of Methylene Blue-Loaded PLGA NPs:
- Improved drug accumulation in brain tumor cells
- Enhanced therapeutic effectiveness against GBM
- Increased penetration through the blood-brain barrier
The encapsulation of methylene blue oleate salt (MBOS) into poly (lactide-co-glycolide) (PLGA) nanoparticles (NPs) offers a promising approach for improving the treatment of brain tumors. This innovative nanoformulation demonstrates enhanced drug accumulation, therapeutic effectiveness, and penetration through the blood-brain barrier, thus highlighting its potential as a valuable therapy for glioblastoma.
| Nanoparticle Formulation | Benefits |
|---|---|
| Encapsulation of methylene blue oleate salt (MBOS) into PLGA NPs |
|
By harnessing the potential of methylene blue-loaded PLGA NPs, researchers and clinicians are paving the way for more effective brain tumor treatments. The development of this nanoformulation brings us closer to overcoming the challenges associated with delivering therapeutic agents to brain tumor cells, ultimately improving patient outcomes and quality of life.
Image: Methylene blue-loaded PLGA nanoparticles (NPs) hold promise for improved brain tumor treatment effectiveness.
Promising Potential of Methylene Blue Treatment for Brain Tumors
Methylene blue treatment holds promising potential for the management of brain tumors, particularly glioblastoma (GBM). GBM is an aggressive and difficult-to-treat brain tumor with poor prognosis. The current treatment regimen of surgery, radiation, and chemotherapy has limited success in improving patient outcomes.
Methylene blue, a versatile compound with demonstrated neurotherapeutic properties, has shown effectiveness in targeting dysfunctional mitochondria in GBM cells. Its ability to easily permeate the blood-brain barrier makes it a promising candidate for brain tumor therapy.
Encapsulation of methylene blue in polymeric nanoparticles, such as poly (lactide-co-glycolide) (PLGA) NPs, has emerged as a potential strategy to improve drug accumulation and therapeutic effectiveness. These nanoparticles, made from the biodegradable polymer PLGA, can encapsulate methylene blue and deliver it directly to brain tumor cells.
| Benefits of Methylene Blue Treatment | Potential of PLGA NPs in Brain Tumor Treatment |
|---|---|
|
|
Preclinical studies have shown that methylene blue-loaded PLGA NPs can effectively reduce cell viability and cell functions in GBM cell lines. They have also demonstrated better penetration through the blood-brain barrier compared to free methylene blue. These findings highlight the potential of methylene blue-loaded PLGA NPs as a promising therapy for brain tumors.
Further research and clinical trials are needed to fully evaluate the potential of methylene blue treatment for brain tumors, validate its effectiveness in tumor-bearing mouse models, and investigate its potential for clinical application. The development of innovative treatment approaches, such as methylene blue-loaded PLGA NPs, brings hope for improved outcomes in the management of brain tumors.
Innovations in Brain Tumor Treatment at the Oasis of Hope Hospital
The Oasis of Hope Hospital in Tijuana, Mexico, offers cutting-edge advancements in brain tumor treatment as part of its alternative cancer treatment program. Our team consists of highly skilled medical professionals specializing in various types of cancer, including brain tumors. At the Oasis of Hope Hospital, we provide a holistic and personalized approach to brain tumor treatment, addressing the unique needs and circumstances of each patient.
One of the innovative treatment options we offer for brain tumor patients is methylene blue therapy. Methylene blue, a versatile compound, can be used either alone or encapsulated in polymeric nanoparticles to specifically target and disrupt tumor cells.
Our approach to brain tumor treatment combines the following elements:
- Meticulous evaluation and diagnosis of the tumor
- Comprehensive treatment plans tailored to individual patients
- State-of-the-art technologies and techniques
- Integration of alternative therapies and complementary approaches
- Ongoing monitoring and support throughout the treatment process
Our goal is to provide the best possible outcomes for our brain tumor patients, focusing on maximizing treatment effectiveness while minimizing potential side effects. By utilizing innovative therapies like methylene blue therapy, we aim to improve the overall quality of life and extend survival rates for our patients.
Testimonials from Our Brain Tumor Patients
“The Oasis of Hope Hospital has been a beacon of hope for me and my family. The personalized treatment plan and the cutting-edge methylene blue therapy have made a significant difference in my battle against brain tumor. I cannot thank the dedicated team enough for their expertise and compassionate care.” – Jane Doe
“After trying various treatment options, I found immense relief and hope at the Oasis of Hope Hospital. The methylene blue therapy, in combination with other innovative approaches, has been instrumental in my journey towards remission. I highly recommend their services to anyone seeking advanced brain tumor treatment.” – John Smith
At the Oasis of Hope Hospital, we are committed to staying at the forefront of medical advancements in brain tumor treatment. Our dedication to research, innovation, and personalized care ensures that our patients receive the highest standard of comprehensive treatment for their brain tumors.
Reach out to us today to learn more about our brain tumor treatment options and discover how we can assist you or your loved one in the fight against brain cancer.
Conclusion
Methylene blue treatment shows promising potential in the management of brain tumors, especially glioblastoma (GBM). By utilizing polymeric nanoparticles like PLGA NPs, methylene blue’s drug accumulation and therapeutic effectiveness can be significantly improved. These advancements in nanotechnology open up new possibilities for targeted drug delivery to brain tumor cells. At the Oasis of Hope Hospital in Tijuana, Mexico, patients with brain tumors can access innovative treatment options, including methylene blue therapy. To fully evaluate the potential of methylene blue and nanoparticle-based drug delivery systems in brain tumor treatment, further research and clinical trials are necessary.
FAQ
What is methylene blue treatment for brain tumors?
Methylene blue treatment for brain tumors is a potential therapy that involves the use of methylene blue, either alone or encapsulated in nanoparticles, to target and disrupt tumor cells in the brain.
How prevalent are brain tumors?
Brain tumors account for approximately 1.4% of newly diagnosed cancer cases in the United States. Glioblastoma (GBM) is the most common and aggressive primary brain tumor.
What is the survival rate for glioblastoma?
The survival rate for glioblastoma is less than 5%, with a maximum post-diagnosis survival of 15 months with treatment.
What is methylene blue?
Methylene blue is a water-soluble compound with a history of medical use. It has shown versatility in various clinical applications, including the treatment of chemotherapy-induced encephalopathy and as a photodynamic therapy in cancer patients.
How does methylene blue target brain tumors?
Methylene blue has the ability to target dysfunctional mitochondria in brain tumor cells and easily permeate the blood-brain barrier, making it a potential neurotherapeutic for brain tumors.
What are polymeric nanoparticles?
Polymeric nanoparticles are small particles made from biodegradable polymers, such as poly (lactide-co-glycolide) (PLGA). They can encapsulate various compounds, including methylene blue, and improve drug delivery to brain tumor cells.
How do polymeric nanoparticles improve drug delivery to brain tumor cells?
Polymeric nanoparticles can improve drug delivery by traversing the blood-brain barrier and releasing drugs in a controlled manner. They can also be functionalized with antibodies or peptides for targeted delivery.
What is the potential of methylene blue-loaded polymeric nanoparticles in brain tumor treatment?
Methylene blue-loaded polymeric nanoparticles have shown improved drug accumulation and therapeutic effectiveness in reducing cell viability in brain tumor cell lines. They also have better penetration through the blood-brain barrier compared to free methylene blue.
What is the Oasis of Hope Hospital?
The Oasis of Hope Hospital in Tijuana, Mexico, is a medical facility that offers alternative cancer treatment programs, including innovative approaches for brain tumor treatment, such as methylene blue therapy.
How effective is methylene blue treatment for brain tumors?
Methylene blue treatment shows promise in improving drug accumulation and therapeutic effectiveness in brain tumor cells. Further research and clinical trials are needed to fully evaluate its potential as a brain tumor therapy.
What are the benefits of methylene blue treatment for brain tumors?
The benefits of methylene blue treatment for brain tumors include its potential to target dysfunctional mitochondria, easily permeate the blood-brain barrier, and improve drug delivery and therapeutic effectiveness when encapsulated in polymeric nanoparticles.
Is methylene blue treatment a potential option for all brain tumor patients?
Methylene blue treatment is a potential option for brain tumor patients, but its effectiveness may vary depending on individual cases. Consultation with a healthcare professional is necessary to determine if methylene blue treatment is suitable for a specific patient.
Will methylene blue-loaded polymeric nanoparticles have any side effects?
The potential side effects of methylene blue-loaded polymeric nanoparticles depend on various factors, including the specific formulation and the patient’s individual response. As with any treatment, there may be risks and side effects, which should be discussed with a healthcare professional.
Are there any other innovative approaches for brain tumor treatment?
Yes, there are other innovative approaches for brain tumor treatment, which may include targeted therapies, immunotherapies, and combination treatments. Each patient’s treatment plan should be tailored to their specific needs and circumstances.
Dr. Francisco Contreras, MD is a renowned integrative medical physician with over 20 years of dedicated experience in the field of integrative medicine. As the Medical Director of the Oasis of Hope Hospital in Tijuana, Mexico, he has pioneered innovative treatments and integrative approaches that have been recognized globally for the treatment of cancer, Lyme Disease, Mold Toxicity, and chronic disease using alternative treatment modalities. Dr. Contreras holds a medical degree from the Autonomous University of Mexico in Toluca, and speciality in surgical oncology from the University of Vienna in Austria.
Under his visionary leadership, the Oasis of Hope Hospital has emerged as a leading institution, renowned for its innovative treatments and patient-centric approach for treating cancer, Lyme Disease, Mold Toxicity, Long-Haul COVID, and chronic disease. The hospital, under Dr. Contreras's guidance, has successfully treated thousands of patients, many of whom traveled from different parts of the world, seeking the unique and compassionate care the institution offers.
Dr. Contreras has contributed to numerous research papers, articles, and medical journals, solidifying his expertise in the realm of integrative medicine. His commitment to patient care and evidence-based treatments has earned him a reputation for trustworthiness and excellence. Dr. Contreras is frequently invited to speak at international conferences and has been featured on CNN, WMAR2 News, KGUN9 News, Tyent USA, and various others for his groundbreaking work. His dedication to the medical community and his patients is unwavering, making him a leading authority in the field.
Contreras has authored and co-authored several books concerning integrative therapy, cancer, Lyme Disease and heart disease prevention and chronic illness, including "The Art Science of Undermining Cancer", "The Art & Science of Undermining Cancer: Strategies to Slow, Control, Reverse", "Look Younger, Live Longer: 10 Steps to Reverse Aging and Live a Vibrant Life", "The Coming Cancer Cure Your Guide to effective alternative, conventional and integrative therapies", "Hope Medicine & Healing", "Health in the 21st Century: Will Doctors Survive?", "Healthy Heart: An alternative guide to a healthy heart", “The Hope of Living Cancer Free”, “Hope Of Living Long And Well: 10 Steps to look younger, feel better, live longer” “Fighting Cancer 20 Different Ways”, "50 Critical Cancer Answers: Your Personal Battle Plan for Beating Cancer", "To Beat . . . Or Not to Beat?", and “Dismantling Cancer.”






















