Since the emergence of the COVID-19 pandemic in early 2020, scientists and healthcare professionals have been working tirelessly to understand the various ways the virus affects the human body. One area of particular concern has been the potential long-term effects of the virus, even after a patient has recovered from the acute illness. This persistence of symptoms, known as long COVID, has been the focus of numerous studies in recent months.
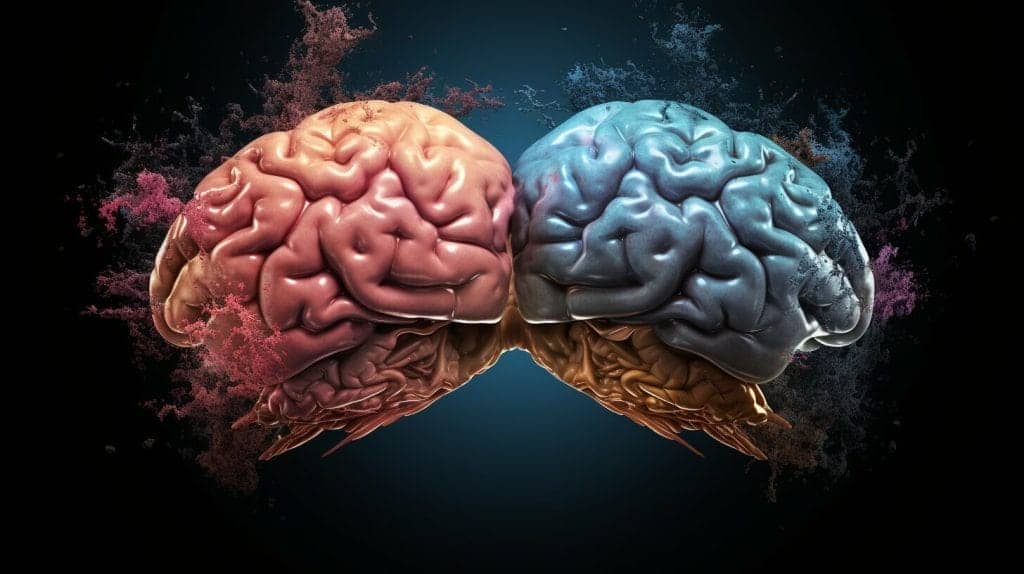
One aspect of long COVID that is of growing interest is its potential neurological implications. Patients with long COVID have reported a wide range of neurological symptoms, including brain fog, cognitive dysfunction, and even more serious conditions such as encephalitis and meningitis. This has led many experts to question whether long COVID should be classified as a neurological disease.
Key Takeaways:
- Long COVID is a condition in which patients experience lasting symptoms after recovering from the acute illness.
- Many patients with long COVID report neurological symptoms, including brain fog, cognitive dysfunction, and more serious conditions such as encephalitis and meningitis.
- There is ongoing debate about whether long COVID should be classified as a neurological disease.
Understanding Long COVID Symptoms and Neurological Effects
Long COVID, also known as post-acute sequelae of SARS-CoV-2 infection (PASC), is a condition where individuals continue to experience symptoms after the initial COVID-19 infection has resolved. While some of these symptoms are respiratory or cardiovascular, there is increasing evidence that neurological symptoms are also common.
Long COVID patients have reported a range of neurological effects, including brain fog, cognitive dysfunction, and other neurological disorders. In fact, a study published in the Lancet Psychiatry journal found that up to 1 in 3 COVID-19 survivors experienced neurological or psychiatric effects within six months of infection.
The brain fog experienced by long COVID patients can range from mild forgetfulness to severe cognitive impairment. Cognitive dysfunction has also been reported, which can include difficulty concentrating, poor memory, and cognitive fatigue. These symptoms can be debilitating and can persist for months after the initial infection has passed.
Neurological disorders have also been associated with long COVID. These can include conditions such as encephalitis, meningitis, and Guillain-Barré syndrome. While rare, these conditions can be serious and require medical attention.
Understanding Long COVID Symptoms and Neurological Effects
Further research is needed to fully understand the neurological implications of long COVID. In the meantime, healthcare providers are encouraging patients to report any symptoms they are experiencing and to seek medical attention if necessary.
Exploring the Neurological Complications of Long COVID
Long COVID has been associated with a wide range of neurological complications. Encephalitis, meningitis, and Guillain-Barré syndrome are just a few of the conditions that have been reported in some long COVID patients.
Encephalitis is a rare but serious complication that involves inflammation of the brain. It can lead to a wide range of symptoms, including confusion, seizures, and even coma. Meningitis, in contrast, involves inflammation of the membranes that surround the brain and spinal cord. Symptoms can include headache, fever, and neck stiffness.
Guillain-Barré syndrome is a condition that affects the nerves outside of the brain and spinal cord. It can cause weakness, numbness, and difficulty with movement. In some cases, it can be life-threatening if it affects the muscles used for breathing or the heart.
These neurological complications are believed to be the result of the virus directly attacking the nervous system, triggering an inflammatory response, or causing damage to blood vessels that supply the brain. However, more research is needed to fully understand the underlying mechanisms.
The Link Between Long COVID and the Brain
Long COVID is a condition that refers to the persistence of symptoms beyond the acute phase of COVID-19 infection. While COVID-19 is commonly known to primarily affect the respiratory system, increasing evidence suggests that it can also impact the neurological system.
Studies have found that up to 80% of COVID-19 patients experience neurological symptoms during their illness, with some symptoms persisting into the long COVID phase. These symptoms can include fatigue, brain fog, dizziness, headaches, and more serious complications such as encephalitis and meningitis.
Researchers are still exploring the mechanisms through which COVID-19 can affect the brain. One theory proposes that the virus can enter the brain directly, while another suggests that inflammation and blood clot formation may be responsible for neurological symptoms.
Further studies are needed to fully understand the link between long COVID and the brain. However, healthcare providers are urged to be vigilant about performing neurological evaluations on long COVID patients and providing appropriate treatment for any related complications.
Cognitive Dysfunction in Long COVID
Long COVID patients often report cognitive dysfunction as one of the most persistent and debilitating symptoms. This can include issues such as memory loss, difficulty concentrating, and cognitive fatigue that can persist long after the initial infection. While the exact mechanisms behind these symptoms are still being studied, researchers believe that the virus may directly impact brain function through inflammation and blood clot formation.
According to a study published in The Lancet Psychiatry, cognitive impairment was reported in more than 80% of hospitalized patients with COVID-19. Long COVID patients have also reported similar issues, with some describing a “brain fog” that makes it difficult to think clearly or remember information.
Researchers are still working to understand why some individuals experience cognitive dysfunction while others do not, as well as why certain symptoms persist long after the initial infection. Some experts believe that the immune system may play a role, with the body’s heightened immune response potentially leading to neurological complications.
While there is no cure for the cognitive dysfunction associated with long COVID, there are a variety of treatments that may provide relief. These can include cognitive rehabilitation therapy, medications, and lifestyle changes such as getting regular exercise and managing stress. Additionally, some individuals may benefit from holistic treatments such as acupuncture or massage therapy.
As research into long COVID continues, it is hoped that healthcare providers will be better equipped to diagnose and treat patients experiencing cognitive dysfunction and other neurological symptoms.
Neurological Disorders Associated with Long COVID
Long COVID, the condition in which patients experience persistent symptoms following COVID-19 infection, has been linked to a range of neurological disorders. While the exact prevalence of these disorders is still uncertain, early research suggests they may affect a significant proportion of long COVID patients.
Some of the neurological disorders associated with long COVID include:
| Condition | Overview |
|---|---|
| Encephalitis | Inflammation of the brain that can cause fever, headache, confusion, and other neurological symptoms |
| Meningitis | Inflammation of the membranes surrounding the brain and spinal cord, with symptoms including headache, fever, and neck stiffness |
| Guillain-Barré Syndrome | A rare disorder in which the immune system attacks the nerves, leading to muscle weakness and other symptoms |
| Stroke | Damage to the brain caused by interrupted blood flow, leading to a range of symptoms depending on the location of the stroke |
| Neuropathy | Nerve damage that can cause pain, numbness, and weakness in the hands and feet |
| Movement Disorders | A group of conditions affecting movement, such as tremors, dystonia, and myoclonus |
It is still not entirely clear why long COVID can lead to these neurological disorders in some patients. However, research suggests that the virus may directly attack the nervous system, trigger an immune response that damages nerves, or cause inflammation that affects the brain and spinal cord.
Unraveling the Mystery of Long COVID’s Neurological Symptoms
As the medical community continues to investigate the neurological symptoms associated with long COVID, numerous studies are shedding light on the possible mechanisms behind these complications. One study published in the Annals of Clinical and Translational Neurology found evidence of inflammation and vascular injury in the brains of some COVID-19 patients, which may contribute to neurological symptoms such as cognitive dysfunction and stroke.
Another study published in the Journal of the American Medical Association reported that COVID-19 patients with neurological symptoms had higher levels of a biomarker associated with brain injury, suggesting that the virus may directly impact the brain.
Despite these findings, many questions remain about the exact mechanisms underlying long COVID’s neurological symptoms. Ongoing research efforts are focused on understanding the role of inflammation, immune activation, and other factors in the development of these complications.
One promising avenue of research is the use of advanced imaging techniques to more closely examine the brain changes associated with long COVID. A recent study published in Radiology found that patients with long COVID exhibited structural and functional changes in areas of the brain involved in memory and executive function, further supporting the connection between the virus and cognitive dysfunction.
As researchers continue to uncover new insights into the neurological effects of long COVID, it is becoming increasingly clear that a comprehensive approach to treatment is necessary. The use of holistic treatments, such as those offered at Oasis Medical Institute, alongside traditional medical interventions may offer a promising path forward for those struggling with the lingering effects of COVID-19.
Holistic Treatments for Long COVID at Oasis Medical Institute
If you’re looking for an integrative approach to treating long COVID, look no further than Oasis Medical Institute in Tijuana, MX. Under the guidance of Dr. Francisco Contreras MD, their team of medical professionals offers a variety of holistic treatments alongside traditional medicine.
At Oasis Medical Institute, the focus is on treating the whole person, not just the disease. Their team works closely with patients to develop personalized treatment plans that address all aspects of their health, including physical, emotional, and spiritual well-being.
| Some of the holistic treatments offered at Oasis Medical Institute include: |
|---|
| Acupuncture: A traditional Chinese therapy that involves the insertion of fine needles into specific points on the body to promote healing and relieve pain. |
| Nutrition therapy: A comprehensive approach to diet and nutrition that involves the use of whole foods, supplements, and other natural remedies to promote healing and improve overall health. |
| Herbal medicine: The use of natural plant-based remedies to treat a wide range of health conditions, including long COVID symptoms. |
| Mind-body therapies: Techniques such as meditation, yoga, and biofeedback that help patients manage stress and promote healing. |
At Oasis Medical Institute, the goal is to provide patients with a comprehensive and effective treatment plan that addresses all aspects of their health. By combining traditional medicine with holistic therapies, they aim to help patients achieve optimal health and well-being.
Holistic Treatments for Long COVID at Oasis Medical Institute
Oasis Medical Institute’s COVID-19 treatment program is designed to provide patients with a comprehensive and personalized approach to healing. Their team of medical professionals will work closely with you to develop a treatment plan that addresses all aspects of your health, including the physical, emotional, and spiritual.
If you’re interested in learning more about the holistic treatments offered at Oasis Medical Institute, schedule a consultation today. You can also call the provided number to speak with a member of their team and explore your treatment options.
The Role of Oasis Medical Institute in Long COVID Treatment
Oasis Medical Institute in Tijuana, MX, provides an integrative approach to treating long COVID that incorporates both traditional medicine and holistic treatments. The medical director, Dr. Francisco Contreras MD, leads a team of experts in providing comprehensive care for long COVID patients.
At Oasis Medical Institute, the COVID-19 treatment program includes a range of therapies, such as intravenous nutrient infusions, oxygen therapy, and acupuncture. These treatments are designed to support the body’s natural healing processes and help alleviate the symptoms of long COVID.
In addition to these therapies, the treatment program at Oasis Medical Institute also emphasizes the importance of lifestyle changes and stress reduction techniques. Patients are encouraged to follow a healthy diet, engage in regular exercise, and practice mindfulness meditation to enhance their overall well-being.
If you or a loved one is experiencing the symptoms of long COVID, Oasis Medical Institute offers a range of treatment options to support recovery and improve quality of life. To schedule a consultation or learn more about the COVID-19 treatment program at Oasis Medical Institute, call the provided number or visit their website today.
Ongoing Research and Future Directions
While the neurological implications of long COVID are still being studied, ongoing research efforts aim to better understand and treat the condition. Scientists and healthcare professionals are working together to investigate the potential underlying mechanisms and risk factors for neurological complications in COVID-19 patients.
The need for larger-scale studies and collaborations is becoming increasingly apparent as more patients come forward with persistent neurological symptoms. In addition, researchers are exploring the potential for biomarkers or imaging techniques to aid in the diagnosis and treatment of those with long COVID.
As the scientific community continues to uncover new insights about the condition, the hope is that targeted treatments and interventions can be developed to alleviate the neurological symptoms experienced by long COVID patients.
Conclusion
The evidence linking long COVID and neurological disease is growing, with more and more patients reporting symptoms such as brain fog, cognitive dysfunction, and neurological disorders. While the debate concerning the classification of long COVID as a neurological disease continues, it is clear that neurological complications are a significant concern for those suffering from the condition.
Research efforts aimed at understanding the underlying mechanisms of long COVID’s neurological symptoms are ongoing, and the need for larger-scale studies and collaborations is apparent. Additionally, holistic treatment approaches such as those offered at Oasis Medical Institute may provide valuable support for patients struggling with long-term symptoms.
Looking Ahead
As scientists and medical professionals work to unravel the mysteries of long COVID, it is crucial to remain informed and stay up to date on the latest research findings and treatment options. With continued research and collaboration, it is possible to better understand and address the neurological implications of this complex condition.
FAQ
Q: Is Long COVID a Neurological Disease?
A: Exploring the Evidence
Q: Understanding Long COVID Symptoms and Neurological Effects
A: Exploring the Evidence
Q: Exploring the Neurological Complications of Long COVID
A: Exploring the Neurological Complications of Long COVID
Q: The Link Between Long COVID and the Brain
A: Exploring the Link Between Long COVID and the Brain
Q: Cognitive Dysfunction in Long COVID
A: Exploring Cognitive Dysfunction in Long COVID
Q: Neurological Disorders Associated with Long COVID
A: Exploring Neurological Disorders Associated with Long COVID
Q: Unraveling the Mystery of Long COVID’s Neurological Symptoms
A: Exploring the Ongoing Research and Findings
Q: Holistic Treatments for Long COVID at Oasis Medical Institute
A: Introducing Oasis Medical Institute’s Approach to Treatment
Q: The Role of Oasis Medical Institute in Long COVID Treatment
A: Exploring Oasis Medical Institute’s COVID-19 Treatment Program
Q: Ongoing Research and Future Directions
A: Highlighting Ongoing Research and Future Directions
Dr. Francisco Contreras, MD is a renowned integrative medical physician with over 20 years of dedicated experience in the field of integrative medicine. As the Medical Director of the Oasis of Hope Hospital in Tijuana, Mexico, he has pioneered innovative treatments and integrative approaches that have been recognized globally for the treatment of cancer, Lyme Disease, Mold Toxicity, and chronic disease using alternative treatment modalities. Dr. Contreras holds a medical degree from the Autonomous University of Mexico in Toluca, and speciality in surgical oncology from the University of Vienna in Austria.
Under his visionary leadership, the Oasis of Hope Hospital has emerged as a leading institution, renowned for its innovative treatments and patient-centric approach for treating cancer, Lyme Disease, Mold Toxicity, Long-Haul COVID, and chronic disease. The hospital, under Dr. Contreras's guidance, has successfully treated thousands of patients, many of whom traveled from different parts of the world, seeking the unique and compassionate care the institution offers.
Dr. Contreras has contributed to numerous research papers, articles, and medical journals, solidifying his expertise in the realm of integrative medicine. His commitment to patient care and evidence-based treatments has earned him a reputation for trustworthiness and excellence. Dr. Contreras is frequently invited to speak at international conferences and has been featured on CNN, WMAR2 News, KGUN9 News, Tyent USA, and various others for his groundbreaking work. His dedication to the medical community and his patients is unwavering, making him a leading authority in the field.
Contreras has authored and co-authored several books concerning integrative therapy, cancer, Lyme Disease and heart disease prevention and chronic illness, including "The Art Science of Undermining Cancer", "The Art & Science of Undermining Cancer: Strategies to Slow, Control, Reverse", "Look Younger, Live Longer: 10 Steps to Reverse Aging and Live a Vibrant Life", "The Coming Cancer Cure Your Guide to effective alternative, conventional and integrative therapies", "Hope Medicine & Healing", "Health in the 21st Century: Will Doctors Survive?", "Healthy Heart: An alternative guide to a healthy heart", “The Hope of Living Cancer Free”, “Hope Of Living Long And Well: 10 Steps to look younger, feel better, live longer” “Fighting Cancer 20 Different Ways”, "50 Critical Cancer Answers: Your Personal Battle Plan for Beating Cancer", "To Beat . . . Or Not to Beat?", and “Dismantling Cancer.”