Welcome to our in-depth exploration of the potential connection between mold toxicity and ulcerative colitis. If you are struggling with ulcerative colitis or are concerned about mold exposure, you’ve come to the right place.
In this section, we will examine the link between mold toxicity and ulcerative colitis, exploring the symptoms of mold exposure and ulcerative colitis, as well as the impact of mold on gut health. We will also examine how to treat and prevent mold exposure to reduce the risk of developing ulcerative colitis. So, let’s dive in to learn more about the fascinating relationship between mold and inflammatory bowel disease.
Understanding Mold Toxicity and Ulcerative Colitis
Mold toxicity and ulcerative colitis are two health issues that may not seem related, but there is evidence to suggest that mold exposure can increase the risk of developing ulcerative colitis. To understand this connection, it’s important to define what mold toxicity and ulcerative colitis are and how they are related.
What is Mold Toxicity?
Mold toxicity, also known as mold illness or biotoxin illness, occurs when exposure to mold and its toxins leads to a range of symptoms and health problems. Mold is a type of fungus that grows in damp, humid environments such as bathrooms, basements, and kitchens. When mold spores are inhaled or ingested, they can cause a variety of health problems.
Some common symptoms of mold toxicity include:
- Coughing and wheezing
- Shortness of breath
- Fatigue
- Headaches
- Muscle pain and weakness
- Memory problems and brain fog
- Insomnia
- Depression and anxiety
In severe cases, mold toxicity can lead to chronic inflammation and damage to the lungs, liver, and other organs.
What is Ulcerative Colitis?
Ulcerative colitis is a type of inflammatory bowel disease (IBD) that affects the lining of the colon and rectum. Symptoms of ulcerative colitis include:
- Abdominal pain and cramping
- Diarrhea, often with blood and mucus
- Frequent bowel movements
- Fatigue
- Weight loss
Ulcerative colitis is thought to be caused by an abnormal immune response to the bacteria that normally live in the gut. This leads to inflammation and ulcers in the colon and rectum.
How are Mold Toxicity and Ulcerative Colitis Related?
While there is still much to learn about the link between mold toxicity and ulcerative colitis, some studies have suggested that mold exposure may increase the risk of developing IBD. One theory is that the toxins produced by mold can disrupt the balance of gut bacteria, leading to inflammation and damage to the lining of the digestive tract.
Another possible explanation is that mold exposure can weaken the immune system, making it more susceptible to infections and autoimmune disorders like IBD.
Regardless of the exact mechanism, it’s clear that mold toxicity and ulcerative colitis are related in some way. This connection underscores the importance of taking steps to reduce your exposure to mold and maintain a healthy gut.
Symptoms of Mold Exposure and Ulcerative Colitis
Mold exposure can cause a variety of symptoms, ranging from mild to severe. When mold exposure is paired with ulcerative colitis, these symptoms can be especially problematic. Here, we will examine the symptoms of mold exposure and ulcerative colitis, and how they can overlap.
Symptoms of Mold Exposure
When exposed to mold, some people may experience respiratory symptoms, such as coughing, wheezing, and shortness of breath. Other common symptoms include skin rashes, itchy eyes, and nasal congestion. In some cases, people may experience digestive issues like abdominal pain, bloating, and diarrhea. However, some people may not experience any symptoms at all.
If you suspect that mold exposure is causing health issues, it is important to schedule an appointment with a doctor to receive a proper diagnosis.
Symptoms of Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease that affects the lining of the colon and rectum. Symptoms can vary from person to person, but may include abdominal pain, diarrhea, rectal bleeding, weight loss, and fatigue. Some people may also experience joint pain and skin rashes.
Ulcerative colitis can be a chronic condition that requires ongoing management, so it is important to speak to a doctor if you suspect that you may be experiencing these symptoms.
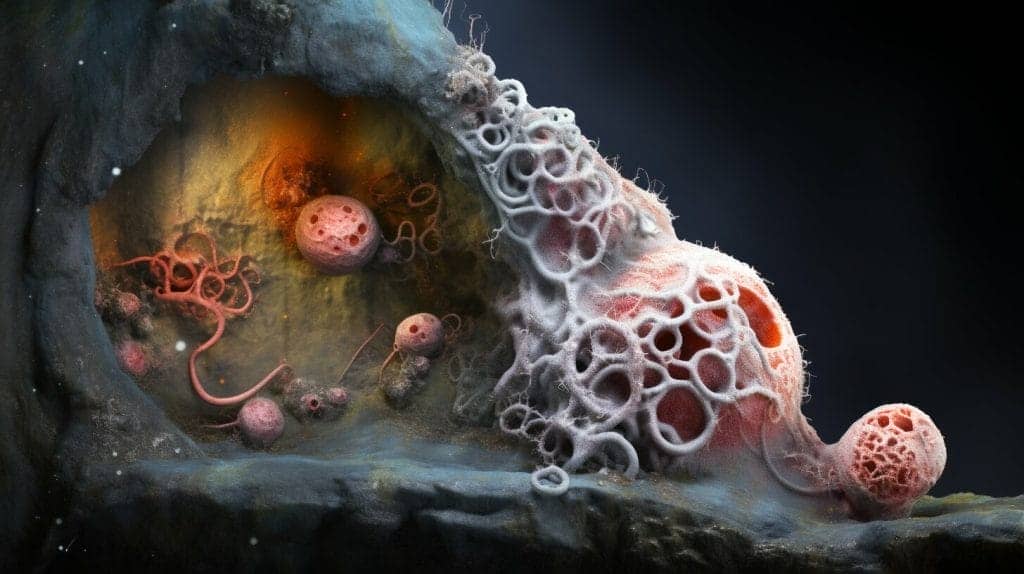
How Mold Affects Gut Health
When mold toxins enter our bodies, they can disrupt the delicate balance of gut bacteria, leading to inflammation and digestive issues. This can cause problems for those with ulcerative colitis, a type of inflammatory bowel disease (IBD).
Studies have shown a link between mold toxicity and IBD, including ulcerative colitis. Mold exposure can trigger symptoms in those with IBD and potentially worsen the condition.
Furthermore, prolonged exposure to mold can lead to a weakened immune system, making it easier for harmful bacteria to grow in the gut. This, in turn, can trigger inflammation and lead to gastrointestinal symptoms.
In addition to disrupting gut bacteria, mold toxins can also damage the intestinal barrier. The intestinal barrier is responsible for preventing harmful substances in the gut from entering the bloodstream. When it is damaged, however, toxins and bacteria can leak into the bloodstream, leading to a variety of health problems.
| Common gastrointestinal symptoms of mold toxicity: |
|---|
| Abdominal pain |
| Diarrhea |
| Bloating |
| Nausea |
It’s important to note that while mold toxicity can worsen symptoms of ulcerative colitis, it is not the root cause of the condition. The cause of ulcerative colitis is still unknown, but it is believed to be a combination of genetic and environmental factors.
The Role of Diet in Managing Mold Toxicity and Ulcerative Colitis
One way to manage the symptoms of ulcerative colitis and mold toxicity is through a healthy diet. Certain foods may trigger symptoms, so it’s important to avoid those. Additionally, incorporating anti-inflammatory foods like leafy greens, berries, and fatty fish may help reduce inflammation in the body.
It’s also important to stay hydrated and to avoid alcohol and caffeine, which can irritate the gut and worsen symptoms.
Diagnosing Mold Toxicity and Ulcerative Colitis
Diagnosing mold toxicity and ulcerative colitis can be challenging because their symptoms are similar to those of other health problems. Doctors use various tests and procedures to identify these conditions, including:
- Blood tests: These tests measure the level of antibodies in your blood to determine if you have been exposed to mold.
- Stool tests: These tests can detect inflammation and infection in your digestive tract.
- Endoscopies: These procedures involve inserting a small camera into your digestive tract to look for signs of ulcerative colitis, such as inflammation and ulcers.
It’s important to note that there is no specific test to diagnose mold toxicity. Instead, doctors rely on a combination of symptoms, medical history, and environmental factors to make a diagnosis.
Treating Mold Toxicity and Ulcerative Colitis
If you have been diagnosed with mold toxicity and ulcerative colitis, it’s important to work with your healthcare provider to determine the best course of treatment. The goal of treatment is to manage symptoms and prevent further complications.
Treating Mold Toxicity
If you have been exposed to mold and are experiencing symptoms, your healthcare provider may recommend one or more of the following treatments:
| Treatment | Explanation |
|---|---|
| Antifungal medication | These drugs are used to kill the fungi that are causing your symptoms. Your healthcare provider may prescribe an oral or topical medication. |
| Decongestants | If you are experiencing nasal congestion or a runny nose, decongestants can help to relieve these symptoms. |
| Corticosteroids | These drugs can help to reduce inflammation in your body and ease symptoms like skin rashes and breathing difficulties. |
| Immunotherapy | If you have a severe allergy to mold, your healthcare provider may recommend immunotherapy. This treatment involves gradually exposing your body to small amounts of the allergen until your immune system becomes desensitized to it. |
In addition to these treatments, your healthcare provider may recommend lifestyle changes to help manage your symptoms. This may include avoiding exposure to mold, using air purifiers in your home, and reducing stress through techniques like meditation or yoga.
Treating Ulcerative Colitis
If you have been diagnosed with ulcerative colitis, your healthcare provider may recommend one or more of the following treatments:
| Treatment | Explanation |
|---|---|
| Anti-inflammatory medication | These drugs can help to reduce inflammation in your gut and relieve symptoms like diarrhea and abdominal pain. |
| Immune system suppressors | If your symptoms are severe, your healthcare provider may recommend drugs that suppress your immune system. This can help to prevent your body from attacking healthy tissues in your gut. |
| Surgery | In some cases, surgery may be necessary to remove the affected portion of your colon and provide relief from symptoms. |
In addition to these treatments, your healthcare provider may recommend dietary changes and lifestyle modifications to help manage your symptoms. This may include avoiding trigger foods, getting regular exercise, and reducing stress.
Preventing Mold Exposure and Ulcerative Colitis
Preventing mold exposure is key in reducing the likelihood of developing ulcerative colitis and other mold-related illnesses.
Reducing Mold Growth in the Home
To reduce mold growth in your home, it is important to:
- Control humidity levels
- Fix leaks promptly
- Ensure proper ventilation in bathrooms and kitchens
- Use dehumidifiers and air conditioners
- Clean and dry any areas affected by water damage
- Regularly clean and disinfect all surfaces
If you suspect that mold is present in your home, it is important to have it tested by a qualified professional. This can help you identify the source of the problem and take steps to remediate it.
Reducing Mold Exposure in Public Spaces
To reduce mold exposure in public spaces, you can:
- Avoid areas that have visible mold growth
- Wear a mask to filter out mold spores
- Use air purifiers and dehumidifiers in enclosed spaces, such as classrooms and offices
- Encourage schools and workplaces to implement measures to prevent mold growth
Additional Measures to Prevent Mold Exposure
In addition to the measures listed above, you can also:
- Regularly clean and replace air filters in your home and car
- Avoid storing clothes and other items in damp or humid areas
- Use mold-inhibiting products, such as paints and cleaning solutions
- Be aware of the signs of mold growth, such as a musty odor and visible discoloration on walls and ceilings
By taking these steps to prevent mold exposure, you can reduce your risk of developing ulcerative colitis and other mold-related illnesses.
The Link Between Mold and Other Health Problems
Mold toxicity can lead to a variety of health problems beyond ulcerative colitis. In this section, we will discuss the other health problems associated with mold exposure.
Asthma and Allergies
Mold exposure can exacerbate asthma and trigger allergies. Mold spores can cause respiratory irritation, leading to coughing, wheezing, and shortness of breath. Those with allergies to mold can experience nasal congestion, itchiness, and sneezing.
Neurological Issues
Mold toxicity can also have neurological effects. Exposure to mold has been linked to memory loss, difficulty concentrating, and mood disorders like depression and anxiety.
Chronic Fatigue Syndrome (CFS)
There has been some research into the link between mold exposure and chronic fatigue syndrome (CFS). Some studies have found that exposure to certain types of mold can lead to symptoms similar to those seen in CFS, such as fatigue, muscle pain, and joint pain.
Mold Toxicity and Children’s Health
Mold exposure can be particularly harmful to children, who are often more vulnerable to the effects of toxins than adults. Children who are exposed to mold may experience a range of health problems, including respiratory issues, developmental delays, and behavioral problems.
How does mold exposure affect children’s health?
When children are exposed to mold, they may experience a variety of symptoms, including coughing, wheezing, and difficulty breathing. Mold exposure has also been linked to the development of asthma in children, a chronic respiratory condition that can make it difficult for kids to breathe. In addition, some studies have suggested that mold exposure may be associated with developmental delays and behavioral problems in children.
Are some children more vulnerable to mold toxicity than others?
Yes, some children may be more vulnerable to the effects of mold exposure than others. For example, children with compromised immune systems or underlying health conditions may be more susceptible to mold-related illnesses. Additionally, children who live in damp or poorly ventilated environments may be at a higher risk of mold exposure.
How can parents protect their children from mold toxicity?
Parents can take a number of steps to reduce their children’s risk of mold exposure. These steps include:
- Keeping the home dry and well-ventilated
- Fixing leaks and other sources of moisture promptly
- Regularly cleaning and disinfecting surfaces in the home
- Using air filters and dehumidifiers to reduce humidity levels indoors
- Encouraging children to wash their hands regularly to reduce their risk of exposure to mold and other toxins
If parents suspect that their children have been exposed to mold, they should contact their healthcare provider to discuss the potential health effects and determine whether any testing or treatment is necessary.
Case Studies: Mold Toxicity and Ulcerative Colitis
Real-life stories can help us understand the impact of mold toxicity on ulcerative colitis patients. Let’s examine a few case studies:
Case Study 1
John was a 42-year-old man who had been diagnosed with ulcerative colitis six years ago. Despite taking medication, he continued to experience abdominal pain, diarrhea, and weight loss. After a thorough examination, his doctor discovered that John’s home was infested with Stachybotrys mold. John’s symptoms improved significantly after he moved out of the contaminated environment and received treatment for mold toxicity.
| Age | Gender | Disease | Mold Type | Treatment |
|---|---|---|---|---|
| 42 | Male | Ulcerative Colitis | Stachybotrys | Antifungal drugs and anti-inflammatory drugs |
Case Study 2
Lisa was a 30-year-old woman who had been living in a damp basement apartment for several years. She was recently diagnosed with ulcerative colitis, but her symptoms continued to worsen despite medication. After a thorough examination, Lisa was found to have a high level of mold toxins in her body. She received treatment for mold toxicity and moved out of the contaminated environment, leading to a significant improvement in her symptoms.
| Age | Gender | Disease | Mold Type | Treatment |
|---|---|---|---|---|
| 30 | Female | Ulcerative Colitis | Various | Antifungal drugs and anti-inflammatory drugs |
Case Study 3
Mike was a 50-year-old man who had been diagnosed with ulcerative colitis ten years ago. Despite taking medication, he continued to experience abdominal pain and diarrhea. After a thorough examination, his doctor discovered that Mike’s workplace was contaminated with mold. Mike received treatment for mold toxicity, and his symptoms improved significantly after he switched to a mold-free work environment.
| Age | Gender | Disease | Mold Type | Treatment |
|---|---|---|---|---|
| 50 | Male | Ulcerative Colitis | Various | Antifungal drugs and anti-inflammatory drugs |
These case studies demonstrate the importance of investigating mold toxicity as a potential cause of ulcerative colitis. If you suspect mold exposure in your home or workplace, seek medical attention and take necessary steps to eliminate the mold, which can contribute to the healing process.
Frequently Asked Questions About Mold Toxicity and Ulcerative Colitis
If you have concerns about mold toxicity and ulcerative colitis, you’re not alone. Here are some frequently asked questions that may help you better understand these conditions:
What are the symptoms of mold exposure?
The symptoms of mold exposure can vary depending on the individual and the type of mold. However, some common symptoms include respiratory problems, skin rashes, and digestive issues like diarrhea and abdominal pain.
How can I tell if I have mold in my home?
Mold can be difficult to detect, especially in the early stages. However, some signs that you may have mold in your home include a musty odor, water damage, and visible signs of mold growth such as discoloration on walls or ceilings.
How can I reduce my exposure to mold?
To reduce your exposure to mold, it’s important to control humidity levels in your home, fix leaks and water damage promptly, and clean and dry any areas affected by moisture. You can also use air purifiers and dehumidifiers to help reduce the risk of mold growth.
Can mold toxicity cause ulcerative colitis?
While the link between mold toxicity and ulcerative colitis is not fully understood, there is evidence to suggest that mold toxins can impact gut health and contribute to the development of conditions like ulcerative colitis and Crohn’s disease.
How is mold toxicity diagnosed?
Mold toxicity can be difficult to diagnose, as many of its symptoms are similar to other health problems. However, doctors may use blood tests, stool tests, and endoscopies to identify the presence of mold toxins in the body.
What treatments are available for mold toxicity and ulcerative colitis?
Treatments for mold toxicity and ulcerative colitis may include medications such as antifungal drugs and anti-inflammatory drugs. Lifestyle changes like diet and exercise can also play a role in managing these conditions.
Can children be affected by mold toxicity?
Yes, children can be affected by mold toxicity, and may be at increased risk for respiratory issues, developmental delays, and behavioral problems as a result of mold exposure.
How can I get treatment for mold-related illness?
If you suspect that you have mold-related illness, it’s important to speak with a doctor. They can help you identify the cause of your symptoms and develop an appropriate treatment plan.
Remember, prevention is key when it comes to mold toxicity and ulcerative colitis. By taking steps to reduce your exposure to mold, you can help protect your overall health and well-being.
Dr. Francisco Contreras, MD is a renowned integrative medical physician with over 20 years of dedicated experience in the field of integrative medicine. As the Medical Director of the Oasis of Hope Hospital in Tijuana, Mexico, he has pioneered innovative treatments and integrative approaches that have been recognized globally for the treatment of cancer, Lyme Disease, Mold Toxicity, and chronic disease using alternative treatment modalities. Dr. Contreras holds a medical degree from the Autonomous University of Mexico in Toluca, and speciality in surgical oncology from the University of Vienna in Austria.
Under his visionary leadership, the Oasis of Hope Hospital has emerged as a leading institution, renowned for its innovative treatments and patient-centric approach for treating cancer, Lyme Disease, Mold Toxicity, Long-Haul COVID, and chronic disease. The hospital, under Dr. Contreras's guidance, has successfully treated thousands of patients, many of whom traveled from different parts of the world, seeking the unique and compassionate care the institution offers.
Dr. Contreras has contributed to numerous research papers, articles, and medical journals, solidifying his expertise in the realm of integrative medicine. His commitment to patient care and evidence-based treatments has earned him a reputation for trustworthiness and excellence. Dr. Contreras is frequently invited to speak at international conferences and has been featured on CNN, WMAR2 News, KGUN9 News, Tyent USA, and various others for his groundbreaking work. His dedication to the medical community and his patients is unwavering, making him a leading authority in the field.
Contreras has authored and co-authored several books concerning integrative therapy, cancer, Lyme Disease and heart disease prevention and chronic illness, including "The Art Science of Undermining Cancer", "The Art & Science of Undermining Cancer: Strategies to Slow, Control, Reverse", "Look Younger, Live Longer: 10 Steps to Reverse Aging and Live a Vibrant Life", "The Coming Cancer Cure Your Guide to effective alternative, conventional and integrative therapies", "Hope Medicine & Healing", "Health in the 21st Century: Will Doctors Survive?", "Healthy Heart: An alternative guide to a healthy heart", “The Hope of Living Cancer Free”, “Hope Of Living Long And Well: 10 Steps to look younger, feel better, live longer” “Fighting Cancer 20 Different Ways”, "50 Critical Cancer Answers: Your Personal Battle Plan for Beating Cancer", "To Beat . . . Or Not to Beat?", and “Dismantling Cancer.”